EATING WHEN YOU
HAVE BEEN UNWELL
Information for patients and their carers
- Do you know that eating a nourishing and balanced diet is important to help us healthy, active and independent?
- What are the main signs & symptoms of unintentional weight loss?
- Can you be overweight and malnourished?
- How can you manage your diet when you have unintentional weight loss?
- What are Oral Nutritional Supplements (ONS)?
- Why have you been prescribed ONS?
- How many ONS do you need to take a day?
- When should you take your ONS?
- What happens if you forget to take it?
- Do you still need to take your ONS if you manage to eat a meal?
- How long should you expect to continue taking your ONS?
- What should you do if you can’t manage or don’t like the ONS you have been prescribed?
- Can I heat them?
- Can I freeze them?
- What should you do if you start to lose weight unexpectedly, or have a poor appetite when you stop taking ONS?
Q. Do you know that eating a nourishing and balanced diet is important to help us healthy, active and independent?
When you are unwell, or recovering from an operation or infection, it can sometimes be hard to eat well. You might not feel like eating, or you may be suffering from symptoms or side effects of your illness, treatment or medications, which can affect your appetite and ability to eat.
This can make it difficult to get enough of what your body needs to recover and could lead you to becoming weaker and having less strength and energy than usual. You may find yourself losing weight, even if you are not trying to do so. Over time, if you do not have enough food to eat, you may unintentionally lose weight and become malnourished. It can also make you more likely to pick up an infection.

Q. What are the main signs & symptoms of unintentional weight loss?
Unintentional weight loss can lead to a reduced quantity of body fat and/ or reduced muscle or bone strength. Healing times and your recovery period may be longer than expected. You may feel tired, have low energy levels or find it hard to keep warm. This in turn could also lead to other effects, such as reduced quality of life, digestive problems or your mood may be affected. Unintended weight loss is one of the key indicators of malnutrition.

Q. Can you be overweight and malnourished?

Undernutrition is usually associated with weight loss. But is highly possible that you are overweight but still suffer from malnutrition, mainly micronutrient malnutrition (deficiency of key micronutrients in diet). Though weight loss in overweight people is seen as a positive aspect, it is important to watch out for unintentional weight loss, no matter what weight you were initially. This weight loss may be due to loss of muscle as opposed to loss of fat, which can further hamper the overall health.
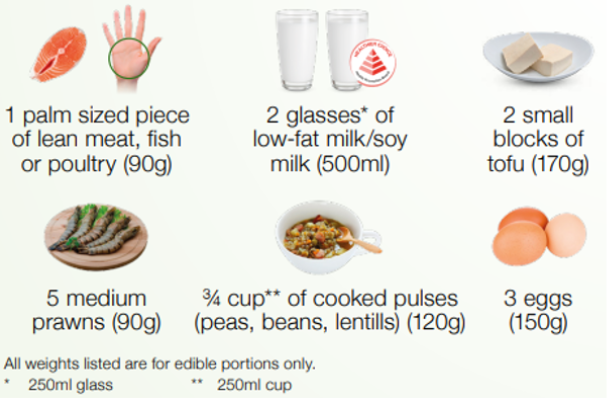
Q. How can you manage your diet when you have unintentional weight loss?
The best way to manage malnutrition is to ensure that your diet contains a balanced mix of nutrients such as macronutrients (energy, protein, fat etc) and micronutrients (vitamins & minerals). However, if you have a poor appetite or are having problems eating due to illness, it can be difficult to obtain all these nutrients from your diet.

Q. What are Oral Nutritional Supplements (ONS)?
Oral Nutritional Supplements (ONS) are supplementary oral intake of dietary food for special medical purposes in addition to the normal food which commonly added with nutrients including carbohydrate, protein, vitamins and minerals. They are usually prescribed by dietitians or doctors to people who have difficulties meeting their daily nutritional needs from food. ONS are one important nutrition intervention strategy for people with poor food intake, low appetite, and those with or at risk of malnutrition.
Q. Why have you been prescribed ONS?
Your healthcare professional (HCP) may feel you could benefit from taking ONS, if they think you require extra nutrition to meet your nutrient needs and you are not able to achieve this through diet alone. If you are unwell, or recovering from an illness, you may need more nutrients than usual due to increased requirements. However, your appetite might be poor and you could struggle to eat and drink enough. If this is the case, your HCP may prescribe ONS to bridge this nutrient gap.

Q. How many ONS do you need to take a day?
ONS can help improve your dietary intake but it is important that you take them every day as recommended by your HCP. Your HCP will explain how many ONS you should take to meet your daily nutritional needs. It is important that you try to take the recommended amount each day, for the recommended length of time, to help you achieve your nutritional goals. If in doubt, you can check with your HCP that issued your prescription.
Q. When should you take your ONS?
In general, people take their ONS when they feel like drinking or eating them. This may be between meals as a snack, first thing in the morning, or before bedtime. Others find it easier to take small amounts regularly throughout the day but try to get into a regular routine and take your ONS at the same time each day. However, please always follow the advice given by your HCP. You should try to avoid using your ONS as a meal replacement, where possible.

Q. What happens if you forget to take it?

In general, you can take your prescribed ONS whenever it’s most convenient for you. If you forget to take it at your normal time, try taking it before bedtime or first thing in the morning. It is important to try and take the recommended amount each day. Speak to your HCP if you are taking medications and have concerns.
Q. Do you still need to take your ONS if you manage to eat a meal?
ONS contains macronutrients and micronutrients such as energy, protein, vitamins & minerals which can help boost your dietary intake. They are designed to be taken in addition to your normal meals so it is important you take the prescribed amount each day between meals, like a snack. If you feel you no longer need them, you should seek the advice of your HCP before stopping your prescribed intake.

Q. How long should you expect to continue taking your ONS?

Your HCP should review and monitor your progress and may agree goals you would like to achieve whilst taking ONS, such as maintaining or gaining weight, increasing energy levels or until you feel able to eat and drink enough to meet your nutritional requirements. They will also assess how long you need to continue taking your ONS.
Q. What should you do if you can’t manage or don’t like the ONS you have been prescribed?
If you are struggling to consume the amount you have been prescribed or are not keen on the flavor you have received, speak to your HCP. There are lots of different styles and flavors of ONS available. Styles include milkshake, juice and dessert style. There is also a wide variety of flavors and volumes.

Q. Can I heat them?
Yes, you can gently warm your ONS especially if you want to add certain flavors to soups, hot drinks, or custard. However do not boil them as you risk destroying some of the nutrients.
Q. Can I freeze them?

Yes, pour the ONS into a freezer-safe container, ice cube tray or ice lolly mould, and freeze. These make a refreshing snack for hot weather or may help to relieve a sore mouth.
Q. What should you do if you start to lose weight unexpectedly, or have a poor appetite when you stop taking ONS?
If you notice changes in your appetite, weight or are unable to eat enough food, discuss your concerns with your HCP as soon as possible. If you have seen a dietitian and they have given you any information, you should take this with you when you visit your HCP next time.